- Edu Soler
- no comments
3D printing (3DP) is a relatively new, rapidly expanding method of manufacturing that found numerous applications in healthcare. Today, it is rapidly expanding: almost every week new printers and printing materials offering novel possibilities as well as new exciting applications appear.
How it works 3DP? 3D printing is a methodology that combines conventional imaging modalities (CT, MRI, Ultrasounds) processed with advanced softwares. The objective is to transform a medical image in a printable file and finally print it. 3D printing requires three procedures; Image Acquisition, Image Processing and three dimensional printing. The common errors in the process are; Under-segmentation skills, sub-optimal transformation into STL file, Sub-optimal image source and Inappropriate 3D printer choice.
This review pretend to give an overview of the most promising trends in differents medical fields and the main stakeholders of the business worldwide.
MEDICAL TRENDS
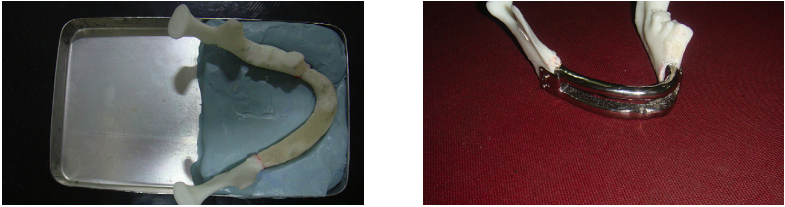
Mandibular prognathism
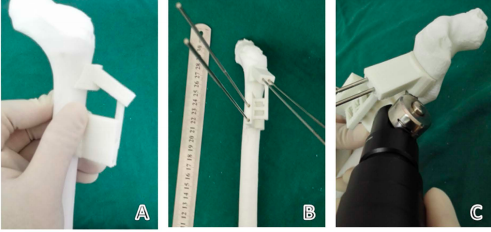
What? Precise Planning of Orthognathic Surgery – Alveolar arches of the maxilla and mandibula of the models were replaced with orthodontic dental cast models. Temporomandibular joints of the models were fixed with Kirschner wire.
Why? To increase of accuracy in orthodontic surgery and prevention of condylar malpositioning and condylar sag by using life-sized, 3D models of our patients preoperatively.
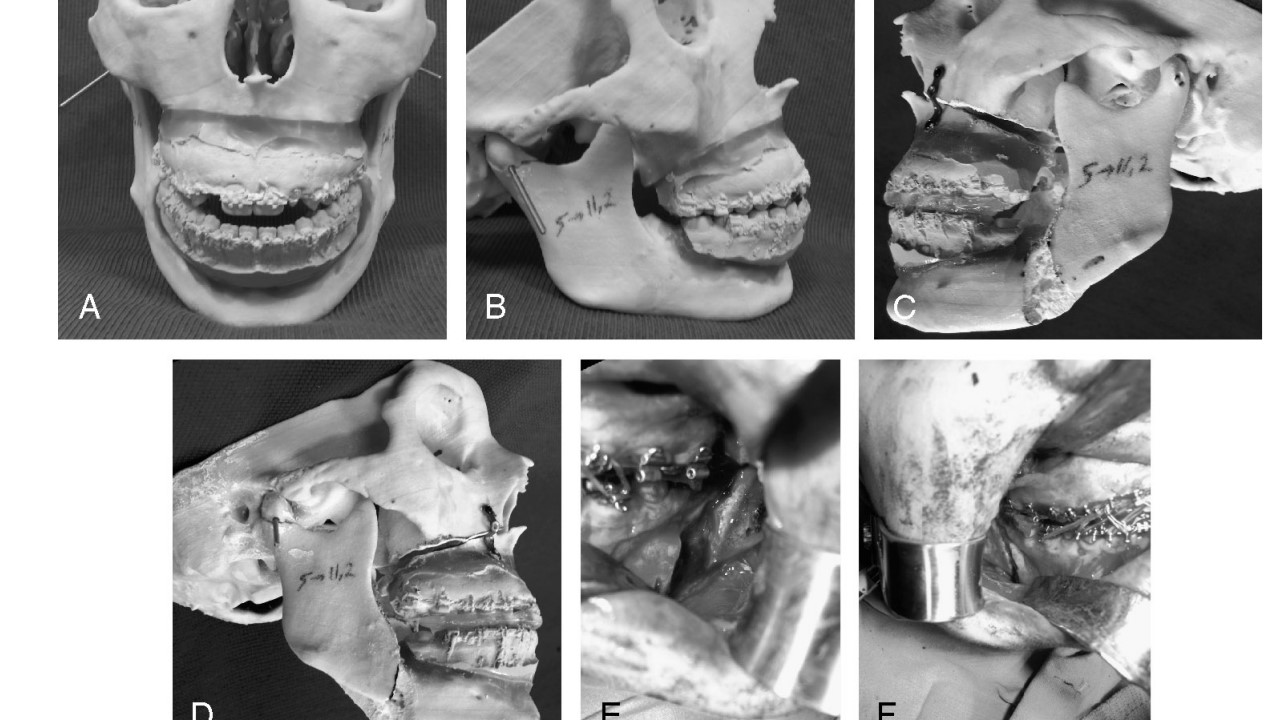
Maxillary retrusion
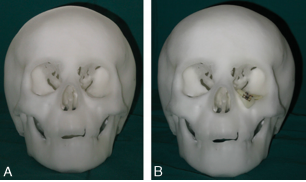
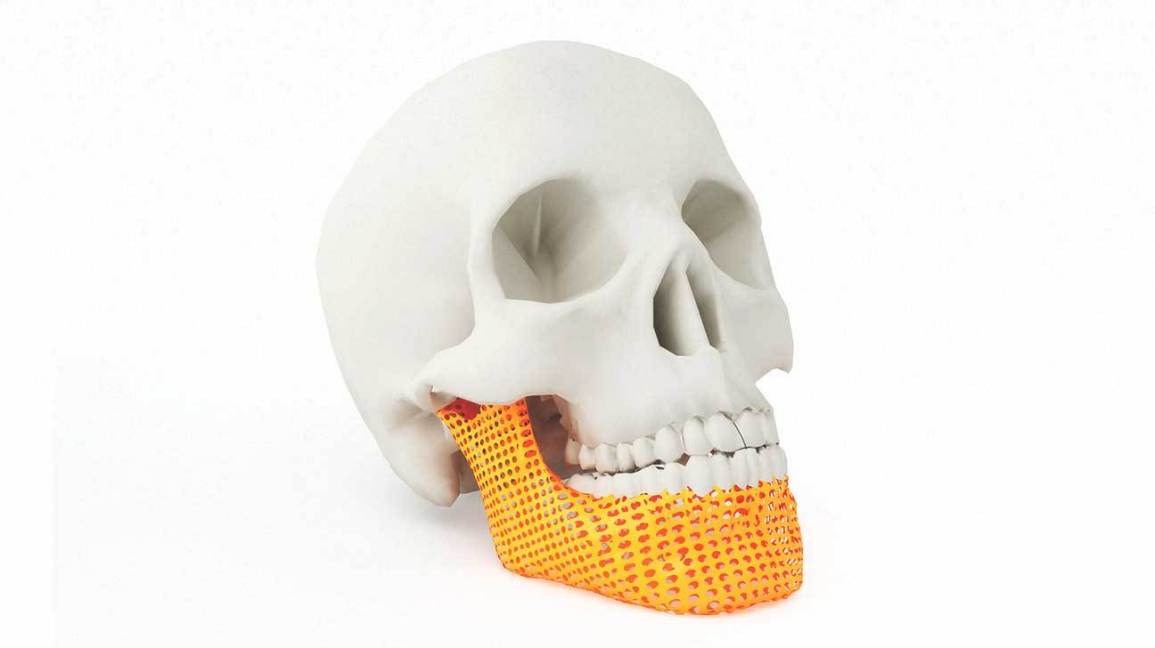
What? Surgical planning, three-dimensional model surgery and preshaped implants in treatment of bilateral craniomaxillofacial post-traumatic deformities.
Why? Accuracy and efficiency and good therapeutic outcomes in the treatment of bilateral craniomaxillofacial post-traumatic deformities.

Orbital floor fractures
What? Models can be used as templates to form titanium mesh implants, which are then used in the reconstruction of orbital floor defects.
Why? Make it easier the process of fitting and aligning implants difficult, time consuming and operator dependent.

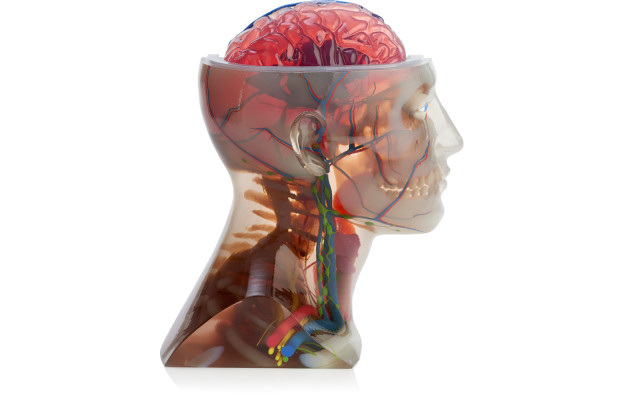
Cerebral tumors
What? Biomodelling in complex surgery in patients with craniofacial, maxillofacial, skull base cervical spinal pathology.
Why? Better communication with patient and other surgeons, help diagnosis and operative planning, and surgeons to rehearse procedures readily.
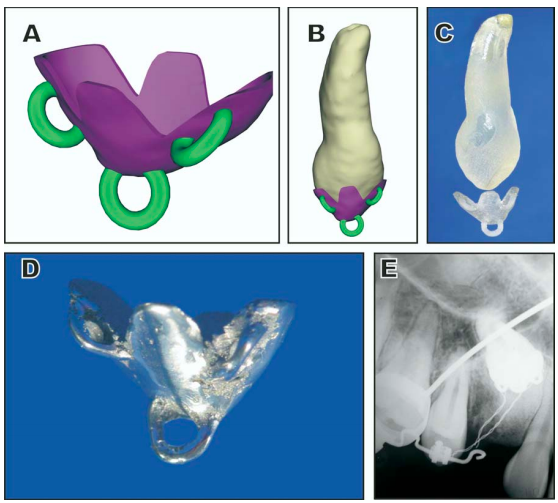
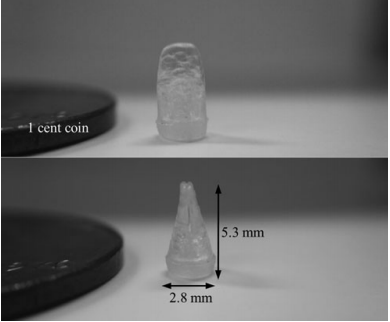
Maxilliary canine impaction
What? Diagnosis and treatment planning of maxillary canine impaction by using computed tomography combined with rapid prototyping.
Why? Treating an impacted maxillary canine requires identifying its exact position; this can pose a challenge to both orthodontists and oral surgeons.
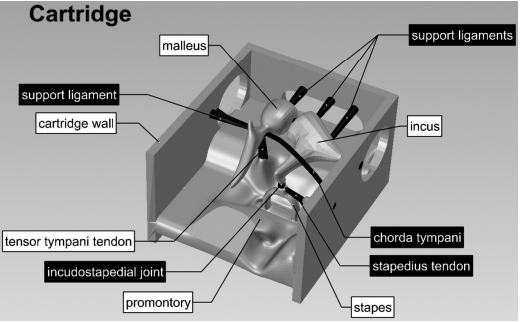
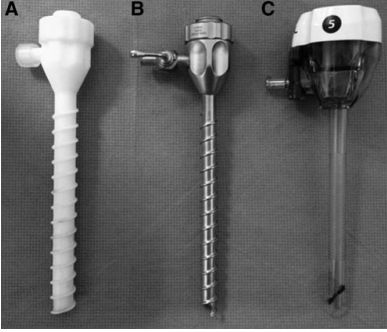
Middle ear diseases
What? A high-fidelity, inexpensive middle ear simulator could be created. Expert otologists will rate the SMS as having a high degree of realism in terms of shape and mechanical properties of the human middle ear affected by otosclerosis.
Why? Inexpensive surgical middle ear simulator enhance surgical training for novice surgeons.
Temporal bone defecte
What? Prototyping of temporal bone for surgical training and medical education.
Why? Scarce availability of temporal bones for trainee.
Facial clefts
What? Mirror technique and rapid prototyping techniques were applied to design and prefabricate the individualized template for the preoperative repair of orbital inferior wall and maxillary anterior wall defects.
Why? Improve surgical accuracy.
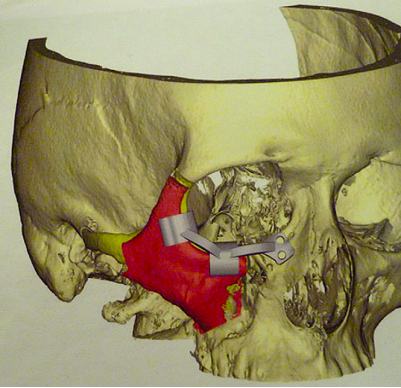
Reposition osteotomy of zygoma
What? Significant reduction in operative time with prototyping in craniofacial surgery: using a positioning guide after zygomatic osteotomy.
Why? The management of post-traumatic deformity in the midface region poses challenges for the maxillofacial surgeon.
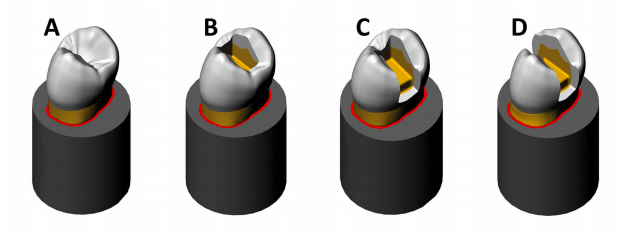
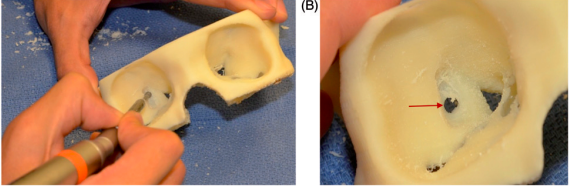
Tooth cavity preparation
What? Operative Dentistry Education – dentistry, where 40 students used 3Dprinted models versus standard schematics and photographs for cavity preparation.
Why? Many students struggle for visual recognition. This is because 2D images and illustrations make it more difficult to identify and view the angles and walls of cavity preparations; also, when the prepare technique is demonstrated by a teacher in real teeth, the students’ field of vision is limited, making it difficult for them to learn.
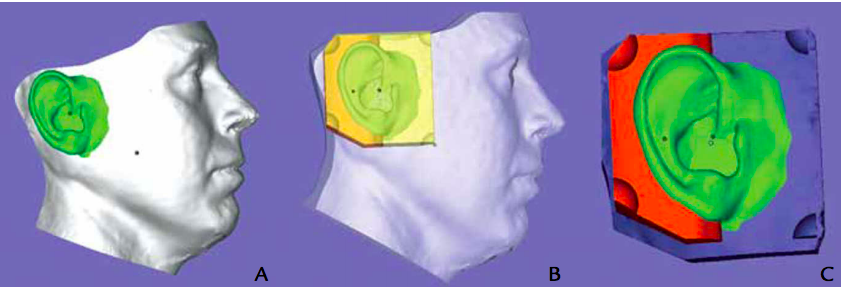
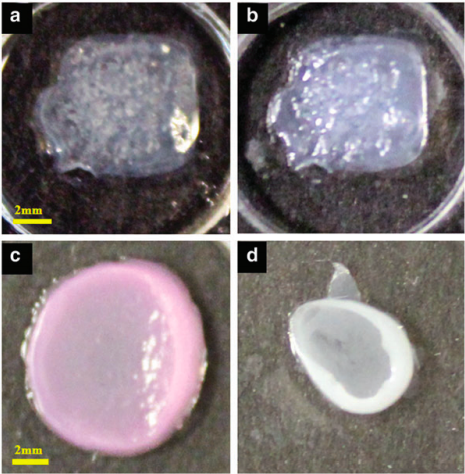
Auricular carcinoma restoration
What? Designing and manufacturing an auricular prosthesis.
Why? Reduce many of the preliminary procedures currently used to create an auricular prosthesis.
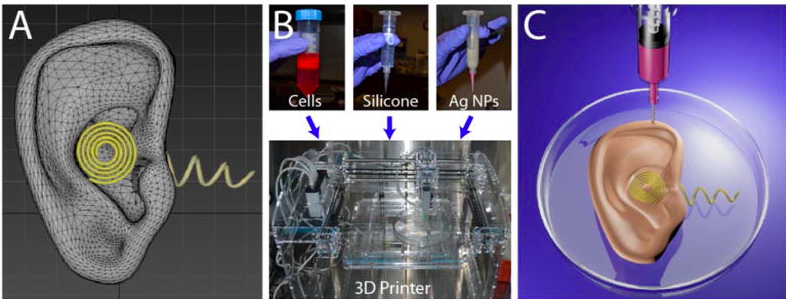
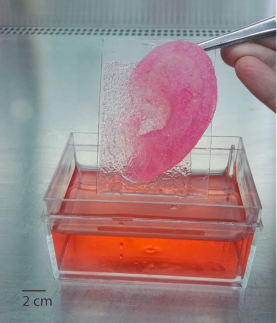
Bionic ear
What? Bionic ear composed of living cells and electronic nanoparticles.
Why? The printed ear exhibits enhanced auditory sensing for radio frequency reception, and complementary left and right ears can listen to stereo audio music. Overall, our approach suggests a means to intricately merge biologic and nanoelectronic functionalities via 3D printing.
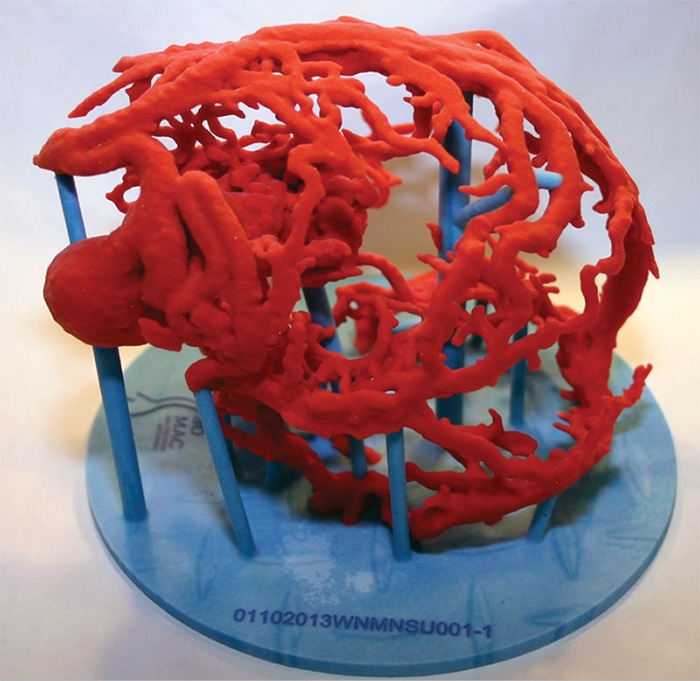
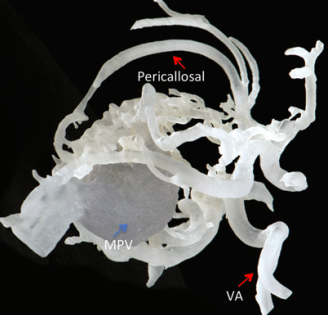
Cerebral aneurysms
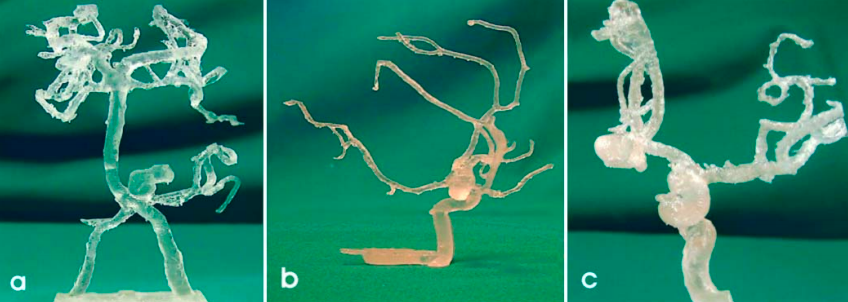
What? Visualization method was used in surgery for cerebral aneurysms. Using the rapid prototyping technology.
Why? The biomodels were used for diagnosis, operative planning, surgical simulation, instruction for less experienced neurosurgeons, and patient education.
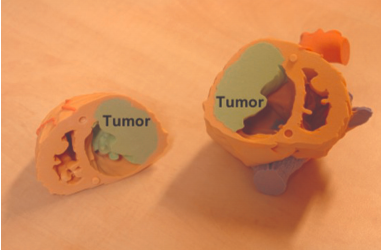
Biomodeling in supracellar mass
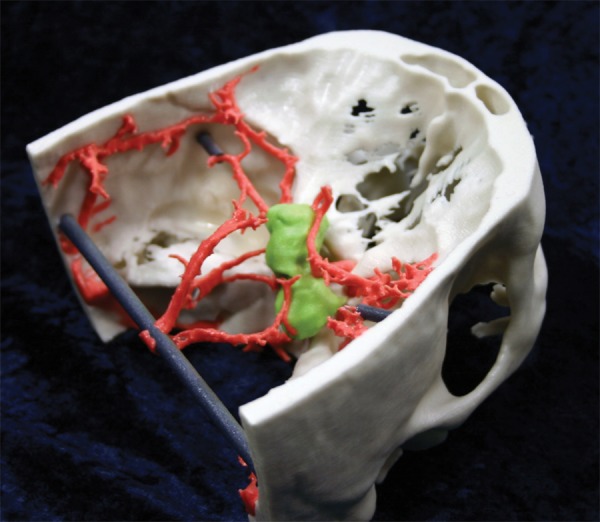
What? Binder jetting 3D-printed model focuses on a suprasellar mass (green).
Why? Relationship between the critical arterial anatomy and bone.
Vascular models
What? Three-dimensional printed vascular models.
Why? Provide unprecedented anatomic and volumetric detail and, in addition to assisting in potential treatment planning, can noninvasively provide details needed to determine a surgical or nonsurgical approach for a complex lesion.
Cerebrovascular aneurysm repair
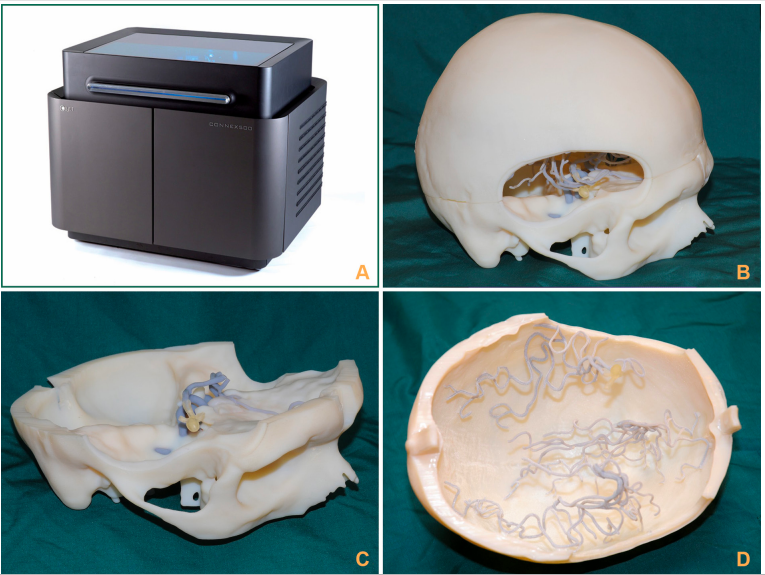
What? Creation of a solid skull and the cerebral vessels in different materials to simulate the real aneurysm when clipped.
Why? Simulation-based training for aneurysm repair.
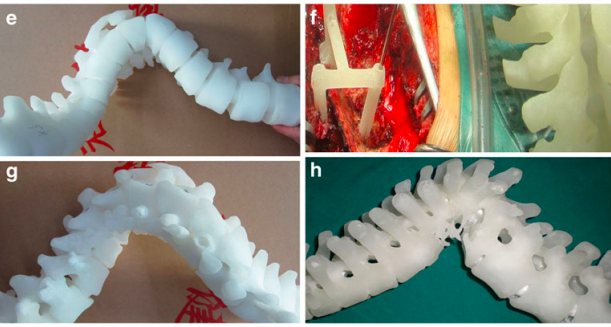
Spinal tumors

What? Surgical training as a learning process for young surgeons or for Ewing’s sarcoma in the cervical spine.
Why? As a result, it is easier for the surgeon to understand the complexity of the case and plan the approach before any surgical procedure.
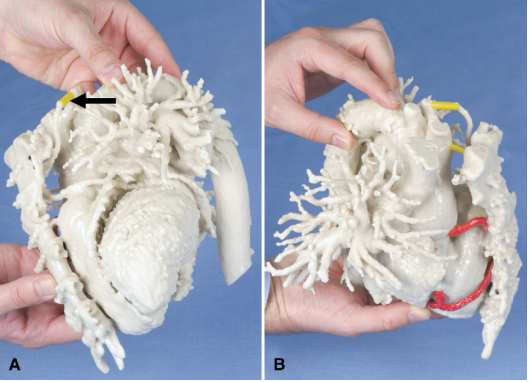
Structural or congenital heart disease
What? Anatomical correct 3D rapid prototyping model (RPT) for patients with complex heart disease and altered geometry of the atria or ventricles.
Why? The use of the 3D rapid prototyping model (RPT-model) during resection of ventricular aneurysm and malignant cardiac tumors may facilitate the surgical procedure due to better planning and improved orientation.
Aortic ulceration
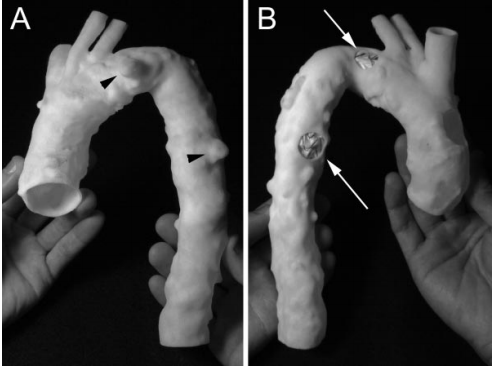
What? Understanding and treating structural heart disease.
Why? Current 2-dimensional imaging techniques remain limited both in their ability to represent the complex 3-dimensional relationships present in structural heart disease and in their capacity to adequately facilitate often complex corrective procedures.
Structural or congenital heart disease?

What? Three-dimensional models of complex congenitally malformed hearts.
Why? Current imaging techniques, however, do not always provide all the necessary anatomic information in a user-friendly fashion.
Aortic valve replacement
What? Surgical planning and intraoperative orientation with 3DP for aortic valve replacement after previous coronary bypass grafting.
Why? Resternotomy for aortic valve replacement in patients with previous coronary artery bypass grafting and an internal mammary artery graft may be a surgical problem.
Pulmonary valve stent implantation
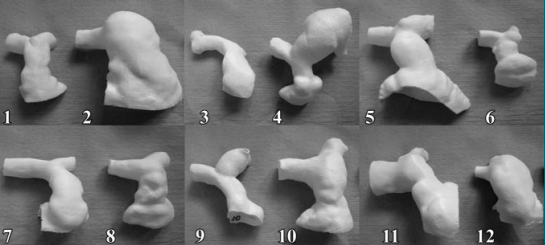
What ? Percutaneous pulmonary valve implantation based on rapid prototyping of right ventricular outflow tract and pulmonary trunk.
Why? Refine the selection of patients for percutaneous pulmonary valve implantation (PPVI).
Simulations of endovascular treatment
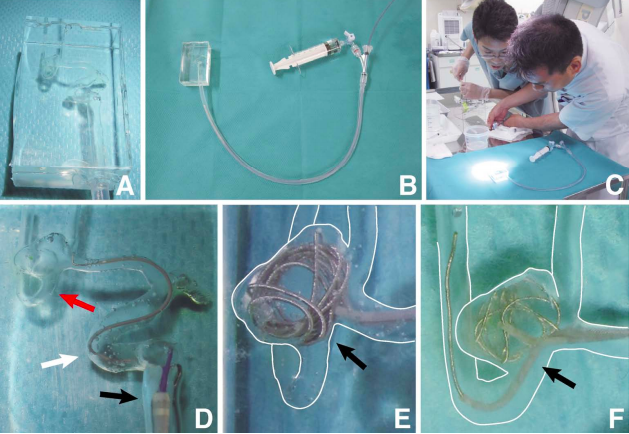
What? Preoperative endovascular simulations in cerebral aneurysm using a patient-specific silicone model.
Why? Simulations are feasible and helpful for designing a treatment strategy and safe manipulation of endovascular devices by experiencing their behavior before actual treatment.
Pulmonary valve stent implantation 2

What? Use of anatomical models for planning of percutaneous pulmonary valved stent implantation.
Why? Allowed the cardiologist’s confidence in patient selection, prosthesis fabrication, and final implantation to be significantly improved.
Model of a severely calcified aorta
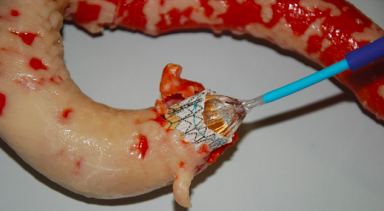
What? Use of three-dimensional printing models for preoperative planning of transcatheter valve replacement in a patient with an extreme porcelain aorta.
Why? Evaluate the potential effects of these constructs for previous surgical planning and simulation of the transcatheter valve replacement.
Aortic stent implantation
What? Use of TangoPlus FullCure 930® is a commercially available rubber-like material that can be used for PolyJet rapid prototyping in the context of experimental cardiovascular modelling.
Why? The appealing possibility of printing models of non-uniform wall thickness, resembling more closely certain physiological scenarios.
Physiology simulation: aorta
What? Rapid prototyping was used to transform aortic geometries as measured by contrast-enhanced MR angiography into realistic vascular models with large anatomical coverage.
Why? Local vascular anatomy and function in the human body is of high interest for the diagnosis and treatment of cardiovascular disease.
Phsyology simulation: coronary
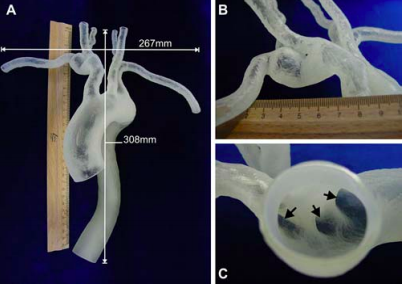
What? Conversion of thoracic aortic vasculature as measured by Magnetic Resonance Imaging into a real physical replica.
Why? Rapid vessel prototyping permits the creation of a concrete solid replica of a patient’s vascular anatomy.
Physology simulation: cerebrovascular
What? Analisis Challenges and limitations of patient-specific vascular phantom fabrication using 3D Polyjet printing.
Why? Anatomic models, for medical device testing and physiological condition evaluation.
Fabrication of cardiac tissue
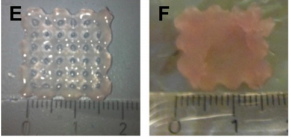
What? Combination of tissue printing technology (TP), human cardiac-derived cardiomyocyte progenitor cells (hCMPCs) and biomaterials to obtain a construct with cardiogenic potential for in vitro use or in vivo application.
Why? With this approach, we were able to generate an in vitro tissue with homogenous distribution of cells in the scaffold. Printing can be used for defined cell delivery, while retaining functional properties.
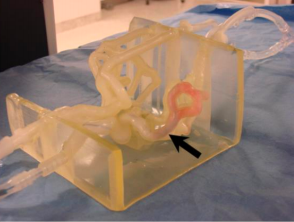
Training transapical aortic replacement

What? Build an appropriate artificial model of the heart that can replace the use of animals for surgical training in trans-apical AVR procedures.
Why? Trans-apical aortic valve replacement (AVR) is a new and rapidly growing therapy. However, there are only few training opportunities.
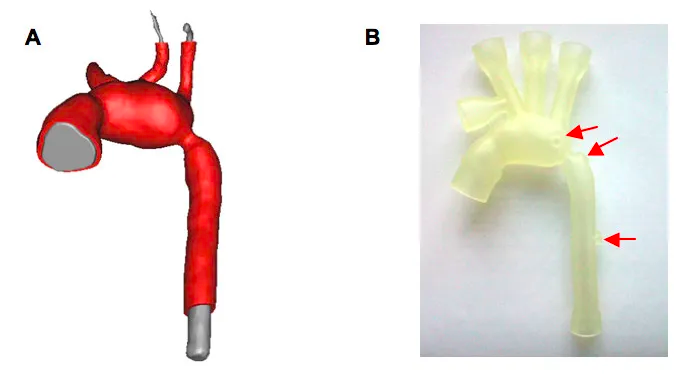
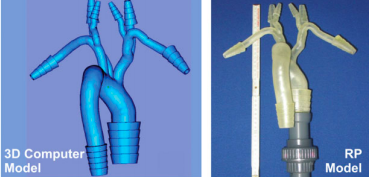
Repair of abdominal aortic aneurysms
What? Three-dimensional (3D) models of AAA using a rapid prototyping technique were developed to help surgical trainees learn how to plan for EVAR more effectively.
Why? The 3D aortic aneurysm model constructed using the rapid prototype technique may significantly improve the ability of trainees to properly plan for EVAR.
Total hip replacement
What? Preoperative planning of this type of surgical interventions due to the possibility of preoperative simulation of the insertion of femoral component into the medullar canal with rapid prototype.
Why? One of the problems we come across in our practice is related to the patients with very disturbed anatomy structures of the hip joint due to the incompatibilities between standard implants and host bone.

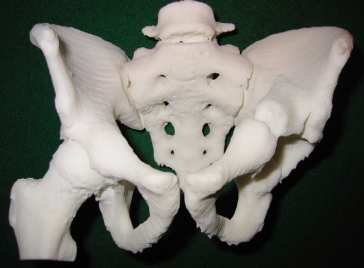
Acetabular fracture
What? The use of medical CT/MRI scanning, three-dimensional reconstruction, anatomical modeling, computer-aided design, RP and computer-aided implantation in treating a complex fracture of acetabulums, calcaneum, and medial condyle of femur (Hoffa’s fracture).
Why? The production of a copy of the fracture or a deformity in a bone with a complex geometry.

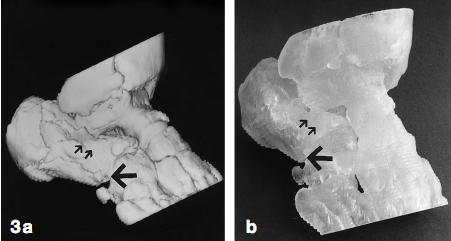
Acetabular fracture 2
What? To evaluate the use of rapid prototyping in the assessment, classification and preoperative planning of acetabular fractures.
Why? The complex three-dimensional anatomy of the pelvis and acetabulum make assessment, classification and treatment of fractures of these structures notoriously difficult.
Intraarticular calcaneal fractures
What? Compare the diagnostic performance of stereolithography vs workstation-based three-dimensional (3D) reformations in intra-articular calcaneal fractures.
Why? Based on our results stereolithograms did not prove to be statistically superior to workstation-based 3D reformations. Stereolithograms may still be useful for teaching purposes and for surgical planning at a thinking-efficacy level.
Scapular osteochondroma
What? A 6 year old girl presented with a large osteochondroma arising from the scapula. Radiographs, CT and MRI were performed to assess the lesion and to determine whether the lesion could be safely resected.
Why? The model allowed better anatomical understanding of the lesion and helped plan surgical management.

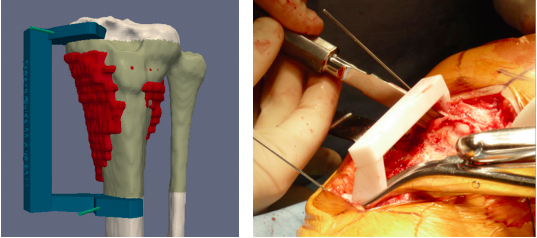
Cubitus varus deformity
What? The aim of this study was to attempt to increase the accuracy of treatment by use of 3-dimensional (3D) computer-aided design. We describe a novel method for ensuring an accurate osteotomy method in the treatment of cubitus varus deformity in teenagers by means of 3D reconstruction and reverse engineering.
Why? Treatment of cubitus varus deformity from a malunited fracture is a challenge. Anatomically accurate correction is the key to obtaining good functional outcomes after corrective osteotomy.
Spinal tumors
What? Surgical training as a learning process for young surgeons or for Ewing’s sarcoma in the cervical spine.
Why? As a result, it is easier for the surgeon to understand the complexity of the case and plan the approach before any surgical procedure.

Charcot foot
What? We depict this method as it pertains to repair of the Charcot foot, it could also be used to plan and practice, or revise, 3-dimensional surgical manipulations of other complex foot deformities.
Why? Charcot foot syndrome (Charcot neuroarthropathy affecting the foot), particularly in its latter stages, may pose a significant technical challenge to the surgeon.

Hip arthroplasty
What? We used specific templates created using a rapid prototyping machine based on the patients’ anatomy, to aid in accurate intraoperative pin placement.
Why? Hip resurfacing arthroplasty (HRA) is a technically demanding operation, requiring both accuracy and precision in placement of the acetabular and femoral components. Malalignment of the component can lead to notching and possible femoral neck fractures.

Distal radius fractures
What? Describe a method for computer-assisted distal radius osteotomies in which computer-generated, patient-specific plastic guides are used for intraoperative guidance.
Why? This allows for unique positioning of the guide during surgery. For each planned drill location, a guidance hole is incorporated into the guide. The guides are easy to integrate into the surgical workflow and minimize the need for intraoperative fluoroscopy for guidance of the procedure.
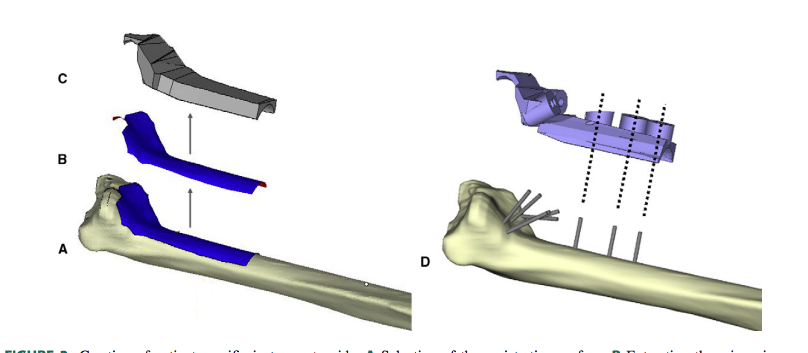
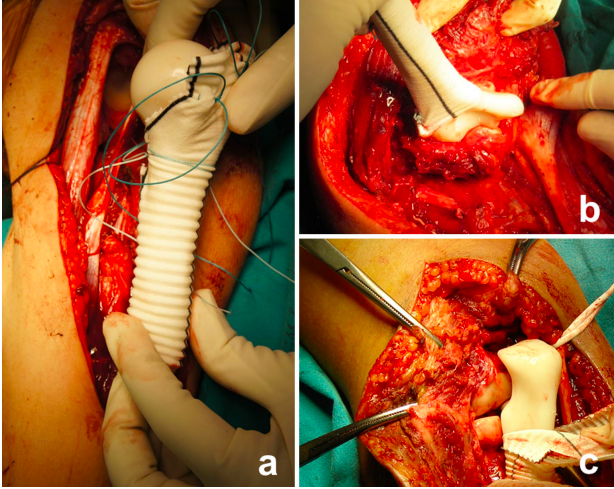
Osteosarcoma resection and allograft reconstruction
What? Surgical guides (patientspecific instruments) for pediatric tibial bone sarcoma resection and allograft reconstruction a method for decreasing the resection margin width and ensuring that the margins are adequate. This method was developed in the tibia, which is a common site for the most frequent primary bone sarcomas in children.
Why? To achieve local control of malignant pediatric bone tumors and to provide satisfactory oncological results, adequate resection margins are mandatory. The local recurrence rate is directly related to inappropriate excision margins.
Thoracic kyphoscoliosis
What? The procedure and results of posterior modified wedge osteotomy aided by the techniques of computer-aided design-rapid prototyping (CAD-RP) to correct thoracic deformities.
Why? The correction of severe thoracic deformities is challenging. However, the usual imaging modalities are not sufficient for performing the surgery
Resection due to bone metastasis
What? To present a rapid-prototype (RP) endoprosthesis replacement after tumor resection in patients with bone metastasis of the upper extremity.
Why? An RP endoprosthesis may have significant advantages when the entire humerus needs to be replaced, or periarticular sites are involved. This technique offers custom-made endoprosthesis with enough durability, and in a relatively short production time at reasonable costs which are suitable for palliative reconstruction.
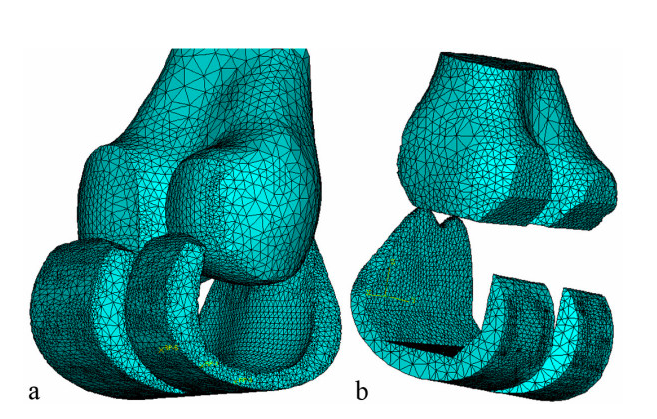
Femoral-component
What? Custom design is based on a Computed Tomography scan of the patient’s joint. The proposed design will customize both the articulating surface and the bone-implant interface to address the most common problems found with conventional knee-implant components.
Why? The longevity of cementless implant components is highly dependent on the initial fit between the bone surface and the implant. The bone-implant interface design has historically been limited by the surgical tools and cutting guides available; and the cost of fabricating custom-designed implant components has been prohibitive.
Maxillofacial defects
What? Rapid prototyping was used as a tool for fabrication of the custommade implant.
Why? Limited visualization of closed internal structures, influence of surgery on airway, presence of teeth and their relationship with the bone, and interference with occlusion often make the surgery complex and unpredictable.
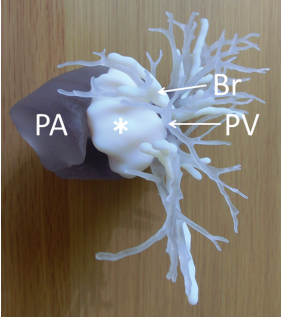
Pulmonary carcinoma
What? Thoracoscopic pulmonary segmentectomy was performed using the fissureless technique simulated by three-dimensional (3D) pulmonary models.
Why? The 3D model and rapid prototyping provided an accurate anatomical understanding of the operative field in both cases. We believe that the construction of these models is useful for thoracoscopic and other complicated surgeries of the chest.
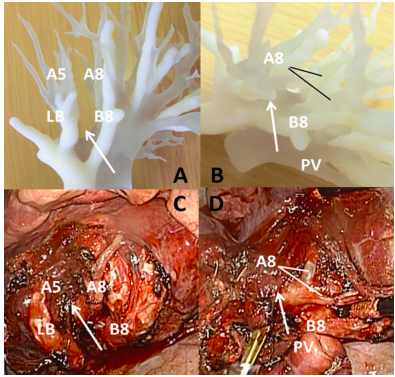
Mediastinal tumors
What? Construction of mediastinal models is useful for thoracoscopic surgery and other complicated surgeries of the chest diseases.
Why? Preoperative three-dimensional (3D) imaging of a mediastinal tumor using two-dimensional (2D) axial computed tomography is sometimes difficult, and an unexpected appearance of the tumor may be encountered during surgery.
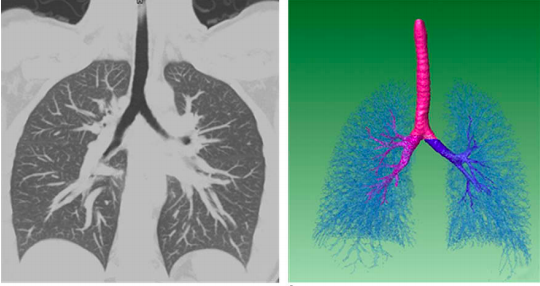
Bronchoscopy
What? Rapid prototyping (RP) technology to create anatomically congruent models of tracheo-bronchial tree for teaching relevant bronchoscopic anatomy.
Why? RP can be successfully used to create anatomically accurate models from imaging studies. There is potential for RP to become a valuable educational tool in the future.

Respiratory flow
What? Three-dimensional image reconstruction by volume rendering and rapid prototyping has made it possible to visualize anatomic structures in three dimensions for interventional planning and academic research.
Why? Using the rapid-prototype model with hyperpolarized helium-3 magnetic resonance imaging show the value of this model for flow phantom studies.
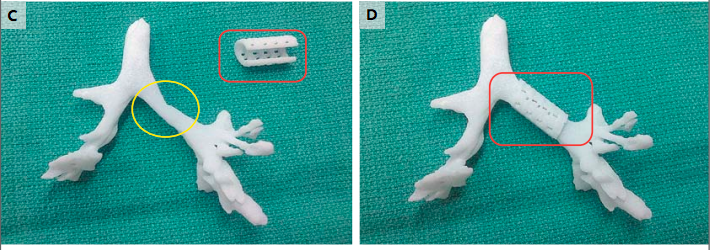
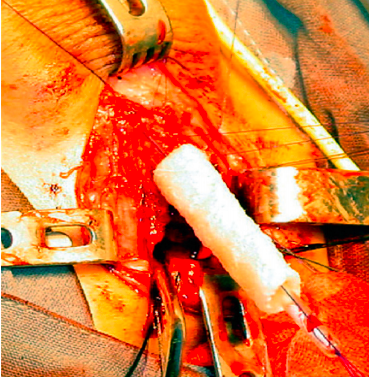
Congenital tracheomalacia
What? In an infant with tracheobronchomalacia, we implanted a customized, bioresorbable tracheal splint, created with a computer-aided design based on a computed tomographic image of the patient’s airway and fabricated with the use of laser-based three-dimensional printing, to treat this life-threatening condition
Why? We reasoned that the localized tracheobronchomalacia was the cause of this physiological abnormality and made a custom-designed and custom-fabricated resorbable airway splint.
Complex congenital abnormalities
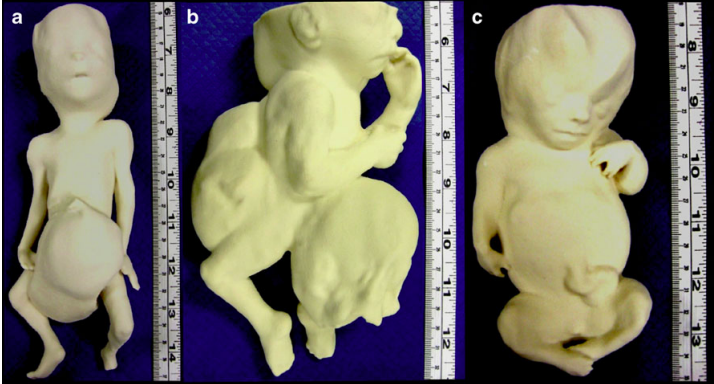
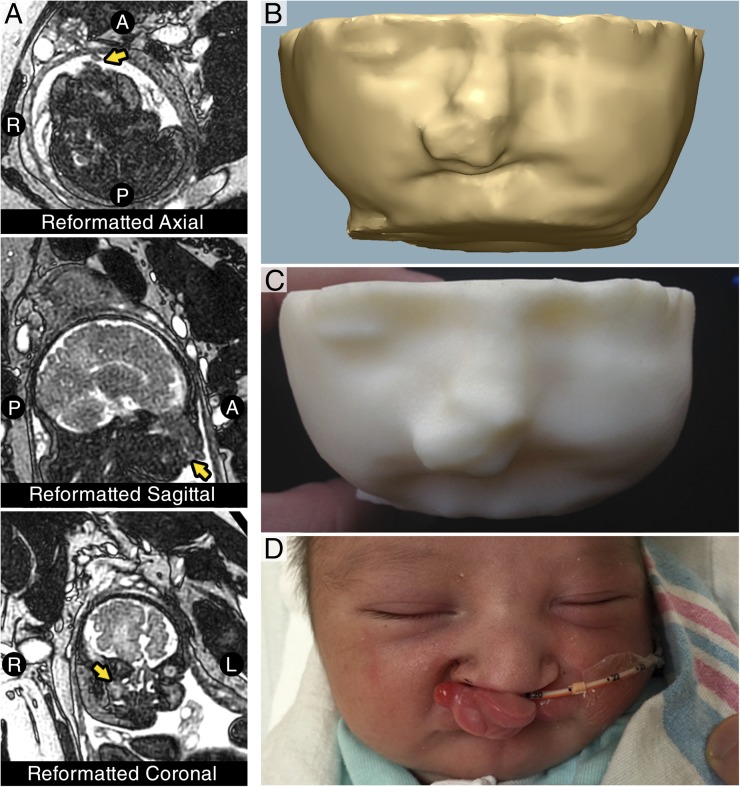
What? Postmortem MR imaging to fabricate 3D-printed models of 11 fetuses and infants and envisioned, among other applications, better understanding of complex congenital abnormalities and opportunities for intrauterine diagnosis and management and more appropriate counseling of parents after pregnancy termination.
Why? The lack of human anatomical material donated for research and training has resulted in issues for medical training
Conjoined twins, skeletal and central nervous system abnormalities, and facial and thoracic defects.
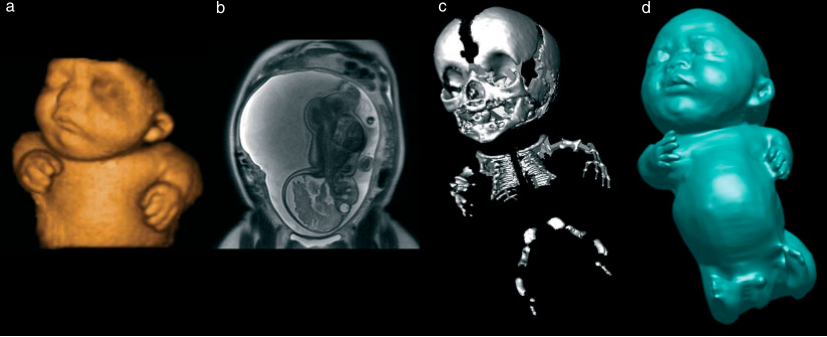
What? To generate physical fetal models using images obtained by three-dimensional ultrasonography (3DUS), magnetic resonance imaging (MRI) and computed tomography (CT) to guide additive manufacturing technology. They were remarkably similar to the postnatal appearance of the aborted fetus or newborn baby, especially in cases with pathology.
Why? The use of 3DUS, MRI and CT may improve our understanding of fetal anatomical characteristics, and these technologies can be used for educational purposes and as a method for parents to visualize their unborn baby.
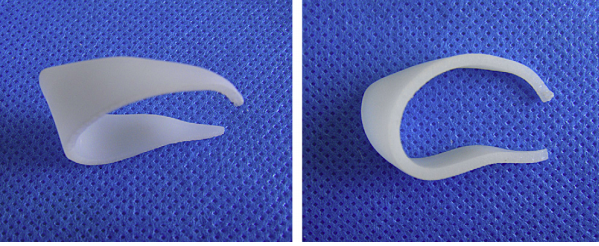
Vaginal dilators

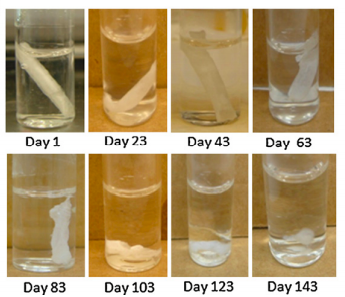
What? We have successfully shown that 3DP can be used to produce vaginal dilators (VD) and vaginal stents (VS) in adult and piglet porcine vaginal tracts.
Why? Currently available VS and VD exist only in adult sizes that cannot be used safely or comfortably in the pediatrics population.
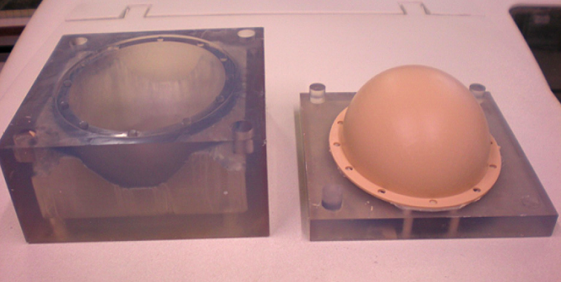
Neonatal head
What? A neonatal head phantom, comprising of an ellipsoidal geometry and including a circular aperture for simulating the fontanel was designed and fabricated,
Why? Allow an objective assessment of thermal rise in tissues during trans-cranial ultrasonic scanning of pre-term neonates.
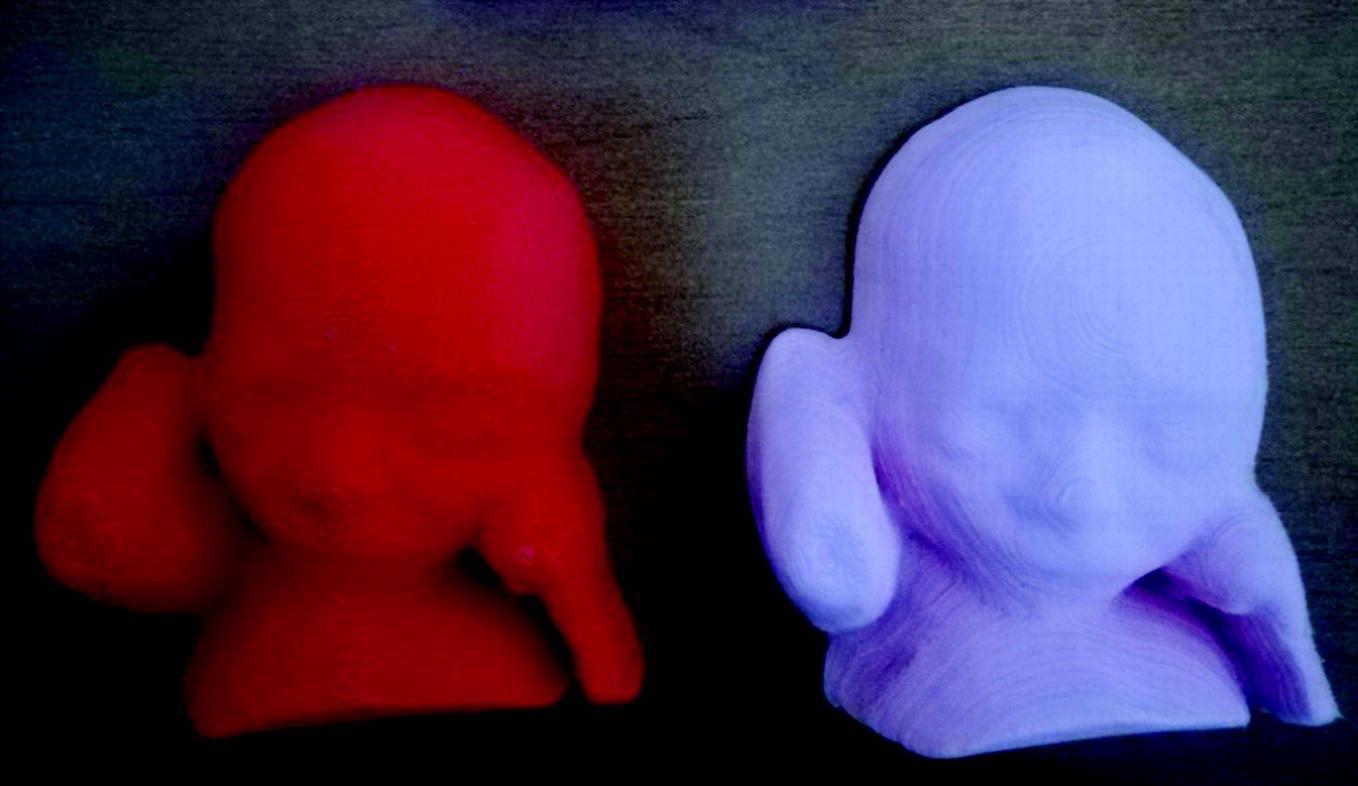
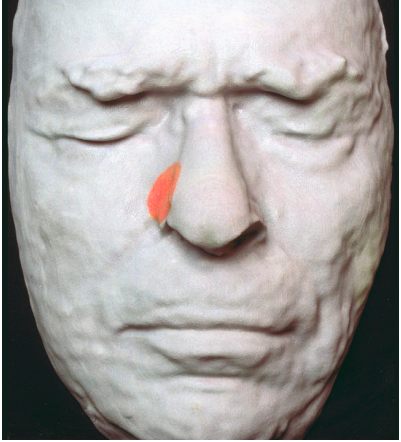
Maternal bonding
What? 3D-printed models of two fetuses with facial clefts.
Why? 3D-printed models can be a useful addition to patient education and can positively impact maternal–fetal bonding.
Cerebrovascular surgery in children
What? 3D printed models of pediatric cerebrovascular lesions
Why? Despite the availability of multiplanar imaging, understanding relational 3D anatomy for complex cerebrovascular lesions can be difficult. 3D printing models provide an instantaneous visualization of lesional anatomy from all perspectives, with the added ability to simulate operative approaches with tactile feedback. The model accuracy using intraprocedural assessment and potential benefit through shortened operative time.
Pediatric Bronchoscopy
What? A Realistic 3D-Printed Tracheobronchial Tree Model from a 1-Year-Old Girl for Pediatric Bronchoscopy Training. Another interesting AM application reported is the prenatal evaluation of complex patient-specific fetal anatomy that was subsequently used to manage complex perinatal airway anomalies.
Why? Because the tracheobronchial tree models used for training to date were scaled for adult lungs, and there is a significant variation between adult lungs and the lungs of a neonate or an infant.

Aberrant Facial Anatomy
What? Evaluation of complex patient-specific fetal anatomy and facilitate the multidisciplinary approach to perinatal management of complex airway anomalies.
Why? The neonate was born with a protuberant cleft lip and palate deformity, without airway obstruction, as predicted by the patient-specific model. Anatomical model, in this case, prevented the surgeons from doing any unnecessary surgical procedure, and the child was discharged without need for airway intervention.
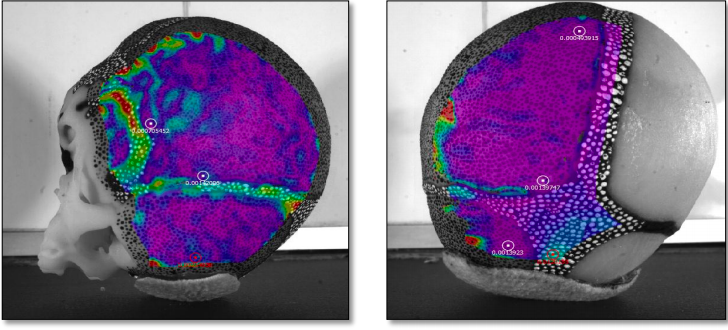
Infant head impact
What? Developed and validated a physical model to investigate the biomechanics of infant head impact, which is the single most common cause of death or permanent disability from injury in children.
Why? Pediatric head injury cause and effect is poorly understood, as the only source of data for such studies have been infant postmortem human surrogates (PMHS).
Dysplasia of the hip
What? Surgical procedure for older children with developmental dysplasia of the hip (DDH).
Why? The use of 3D-printed navigation templates resulted in reduced operation time, decreased intraoperative X-ray exposure and surgical risk, reduced epiphysis damage, as well as better operative guidance and surgical precision.
Uveal melanomas
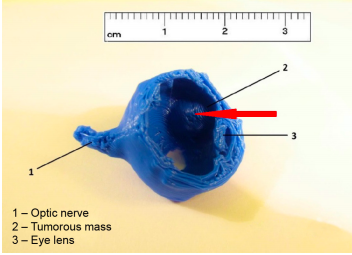
What? The objective of this study was to determine the use of 3D printed model of an eye with intraocular tumor for linear accelerator-based stereotactic radiosurgery.
Why? The 3D printed model of eye with tumor was helpful in planning the process to achieve the optimal scheme for irradiation which requires high accuracy of defining the targeted tumor mass and critical structures.
Surgical training
What? 3D orbit models for use in orbital surgical training using 3D printing technology.
Why? These models allow trainee surgeons to perform ‘wet-lab’ orbital decompressions and simulate upcoming surgeries on orbital models that replicate a patient’s bony anatomy.
Secondary Orbital Reconstructions
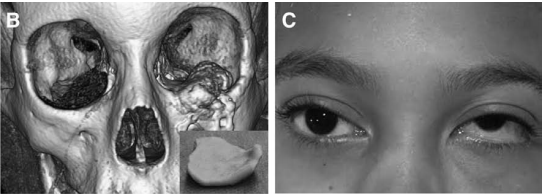
What? Feasibility and accessibility of low-cost, independent use of 3D printing technology to fashion patient-specific implants in orbital reconstruction.
Why? The authors report the technique of low-cost 3D printing of orbital implant templates used in complex, often secondary, orbital reconstructions.
Smartphone fundoscopy
What? Simple technique of fundus photography in human and rabbit eyes using a smartphone.
Why? An inexpensive app for the smartphone, and instruments that are readily available in an ophthalmic practice.
Bioartificial livers
What? A case study about the Viability in the creation of a artificial liver using Rapid prototyping (RP) technologies.
Why? These technologies might eventually enable the manufacture of human livers to create functional substitutes for treating liver failure or dysfunctionalit. However, the approaches used currently face many challenges, such as the complex branched vascular and bile ductular systems and the variety of cell types, matrices and regulatory factors involved in liver development.
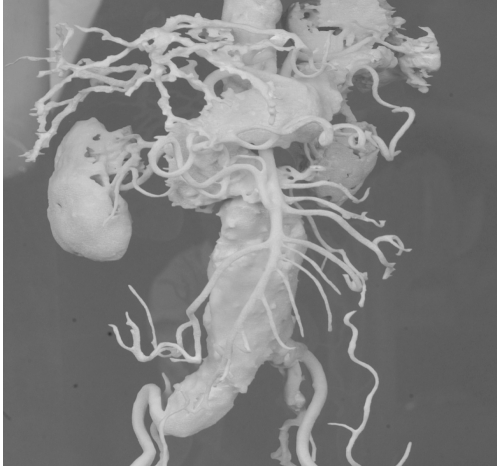
Liver transplant surgery

What? Three-dimensional printed models of the liver plus vascular and biliary structures assisted in preoperative planning and intraoperative orientation in three living-donor liver transplant surgeries. Using standardized preoperative, intraoperative, and postoperative assessments, it is demonstrated identical anatomical and geometrical landmarks in the 3D-printed models and native livers.
Why? Ensuring the safety of donors and recipients is critical. The preoperative identification of the vascular and biliary tract anatomy with 3-dimensional (3D) printing may allow better preoperative surgical planning, avert unnecessary surgery in patients with potentially unsuitable anatomy, and thereby decrease the complications of liver transplant surgery.
Liver transplant surgery 2
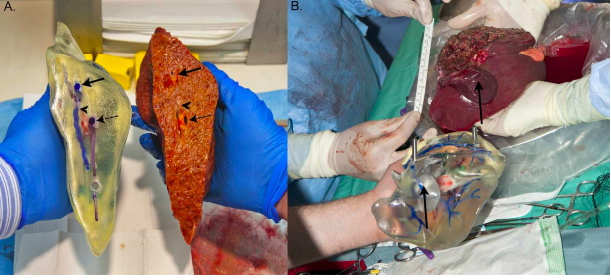
What? The preoperative identification of the vascular and biliary tract anatomy with 3‐dimensional (3D) printing.
Why? Better preoperative surgical planning.
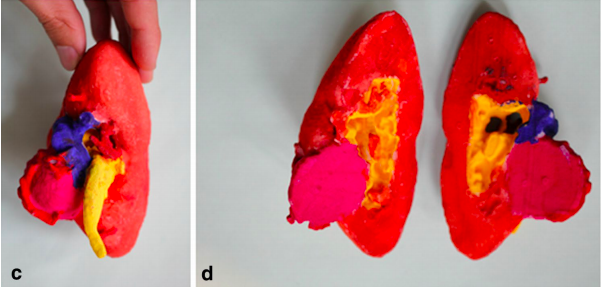
Renal tumor
What? 3D printed the kidneys plus a renal tumor in five patients who were candidates for partial nephrectomy .To construct high-fidelity, patient customized, physical, 3-dimensional (3D) models of renal units with enhancing renal lesions identified on cross-sectional imaging.
Why? Aid patients, trainees, and clinicians in their comprehension, characterization, localization, and extirpation of suspicious renal masses.
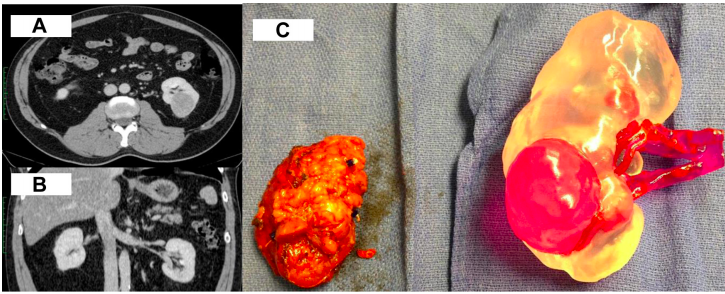
Laparoscopic partial nephrectomy
What? Objectives To investigate the impact of three-dimensional (3D) printing on the surgical planning, potential of training and patients’ comprehension of minimally invasive surgery for renal tumors.
Why? Generating kidney models of T1N0M0 tumors with 3D printing are feasible with refinements to be performed. Face and content validity was obtained when those models were presented to experienced urologists for making practical planning and training. Understandings of the disease and procedure from patients were well appreciated with this novel technology.
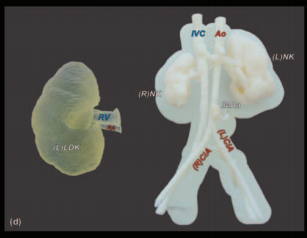
Pediatric Renal Transplantation
What? The authors investigated a novel application of patient-specific three-dimensional (3D) printing, to enhance preoperative, multidisciplinary planning in complex, living-donor pediatric renal transplantation.
Why? We report the new and safe integration of patient-specific 3D printing into complex pediatric renal transplantation. This technique enhances surgical planning and can inform operative feasibility in those cases which would otherwise be uncertain.
Training percutaneous nephrolithotomy
What? A training model to improve technique and understanding of renal anatomy could improve complications related to renal puncture; however, no model currently exists for resident training.
Why? Percutaneous nephrolithotomy (PCNL) is a popular method to remove kidney stones; however, broader use by the urologic community has been hampered by the morbidity associated with needle puncture to gain access to the renal calix (bleeding, pneumothorax, hydrothorax, inadvertent colon injury).

Ureteral stents
What? One-way antireflux valves for ureteral stents.
Why? The 3D printing take advantage of an effective miniaturization, and high level of precision and reproducibility to generate one-way valves for ureteral stents to reduce retrograde flow of urine.
Trocars for laparoscopic
What? Trocars for laparoscopic surgery have also been manufactured by 3D printing to test the utility of printed surgical equipment to reduce waste and solve potential issues of instruments not being available when needed.
Why? In this pilot study, 3D printing of ureteral stents and trocars is feasible, and these devices can be deployed in the porcine and cadaver models. Three-dimensional printing is rapidly advancing and may be clinically viable in the future.
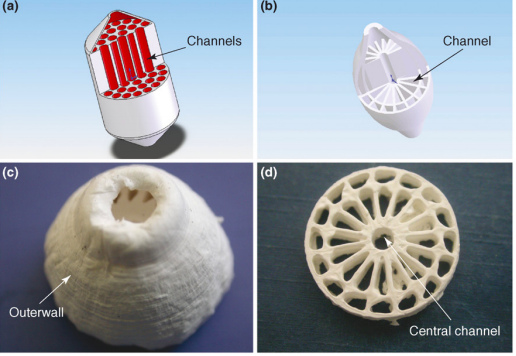
Uretra treatment scaffolds
What? 3D printing allows to construct onto schaffold in which functional cells of the target organ are printed in a second overlying layerthe. These scaffold should eventually degrade and be replaced by extracellular matrix proteins produced by the functional cells.
Why? Local treatment administration.
Skin cancer treatment
What? The use of a customized radiation shield that combines tissue-equivalent bolus material with protective material addresses these issues using rapid prototyping to design and fabricate an extraoral radiation shield. This innovative application provides an expedient, standardized approach for delivering radiotherapy to the face, which is not only more comfortable for the patient, but allows more precise treatment delivery.
Why? Radiation therapy for the treatment of head and neck skin cancer poses challenges because of the inherently uneven tissue topography of the face and the need to protect surrounding unaffected tissues.
Printed skin tissue
What? Flexible automated on-demand platform for the free-form fabrication of complex living architectures
Why? 3D bioprinting offers several advantages in terms of shape- and form retention, flexibility, reproducibility, and high culture throughput. It has a broad range of applications in transdermal and topical formulation discovery, dermal toxicity studies, and in designing autologous grafts for wound healing.
Complete skin model
What? The focus of the present study is to demonstrate the capability of a newly developed ink formulation and the use of an open source printer, for the production of a really complete skin model.
Why? Organ in vitro synthesis is one of the last bottlenecks between tissue engineering and transplantation of synthetic organs. Bioprinting has proven its capacity to produce 3D objects composed of living cells but highly organized tissues such as full thickness skin (dermis + epidermis) are rarely attained.
Epidermal Electronics
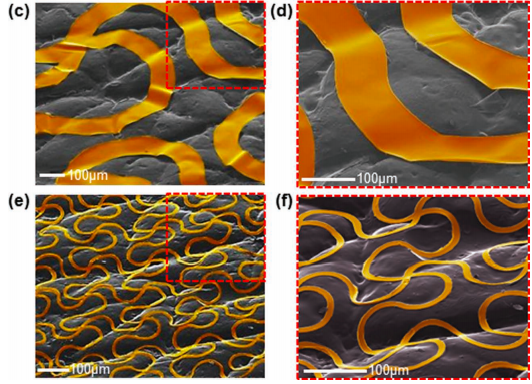
What? Multifunctional Epidermal Electronics Printed Directly Onto the Skin. Materials and designs are presented for electronics and sensors that can be conformally and robustly integrated onto the surface of the skin.
Why? A multifunctional device of this type can record various physiological signals relevant to health and wellness. This class of technology offers capabilities in biocompatible, non‐invasive measurement that lie beyond those available with conventional, point‐contact electrode interfaces to the skin.
Compliance for pediatric patients
What? Since the printer software allows the creation of shapes with equivalent volume, tablets of different shape but containing the same dose, can be printed.
Why? Printing tablets in different shapes and colors to the liking of the child is expected to increase compliance for pediatric. It is also important to note that the shape of the tablet affects many other attributes including the disintegration and rate of dissolution or rate of drug release.
Local drug delivery in catheter and devices
What? Medical implants and devices, such as stents and catheters, are treated with active solutions or suspensions for local drug delivery, usually by coating or spray-coating techniques.
Why? 3D printing offers increased efficiency, spatial and volume control for the treatment process.

SPRITAM levetiracetam
What? SPRITAM®, an FDA-approved 3D-printed drug, has a unitary porous structure produced by a 3D printing process that binds powders without compression. This structure allows tablets with up to 1000 mg of levetiracetam to disintegrate within seconds when taken with a sip of water.
Why? The U.S. Food and Drug Administration (FDA) approved Aprecia Pharmaceuticals Company’s 3D-printed SPRITAM levetiracetam for oral use in treating epileptic seizures recently. The prospect of tailor-made drugs that are customized to individual patient need.

Levofloxacin
What? A 3D printing monolithic implants of levofloxacin.
Why? The printed implants showed more porous infrastructure than those prepared by compression; thus, the drug release from the printed implant showed faster and slightly higher burst release than the compressed dosage form18. The implants printed with an inner drug reservoir and inner and outer drug layers were able to show pulsed and bimodal drug release.

Dexamethasone-21- phosphate disodium salt
What? A novel extrusion printing system was used to create drug delivery structures wherein dexamethasone-21-phosphate disodium salt (Dex21P) was encapsulated within a biodegradable polymer (PLGA) and water soluble poly(vinyl alcohol) (PVA) configurations
Why? This approach clearly demonstrates that the extrusion printing technique provides a facile and versatile approach to fabrication of novel drug delivery platforms.
MOST RELEVANT STAKEHOLDERS
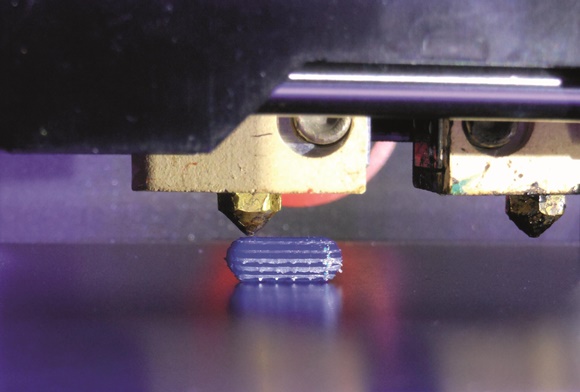
Melting of hard filaments
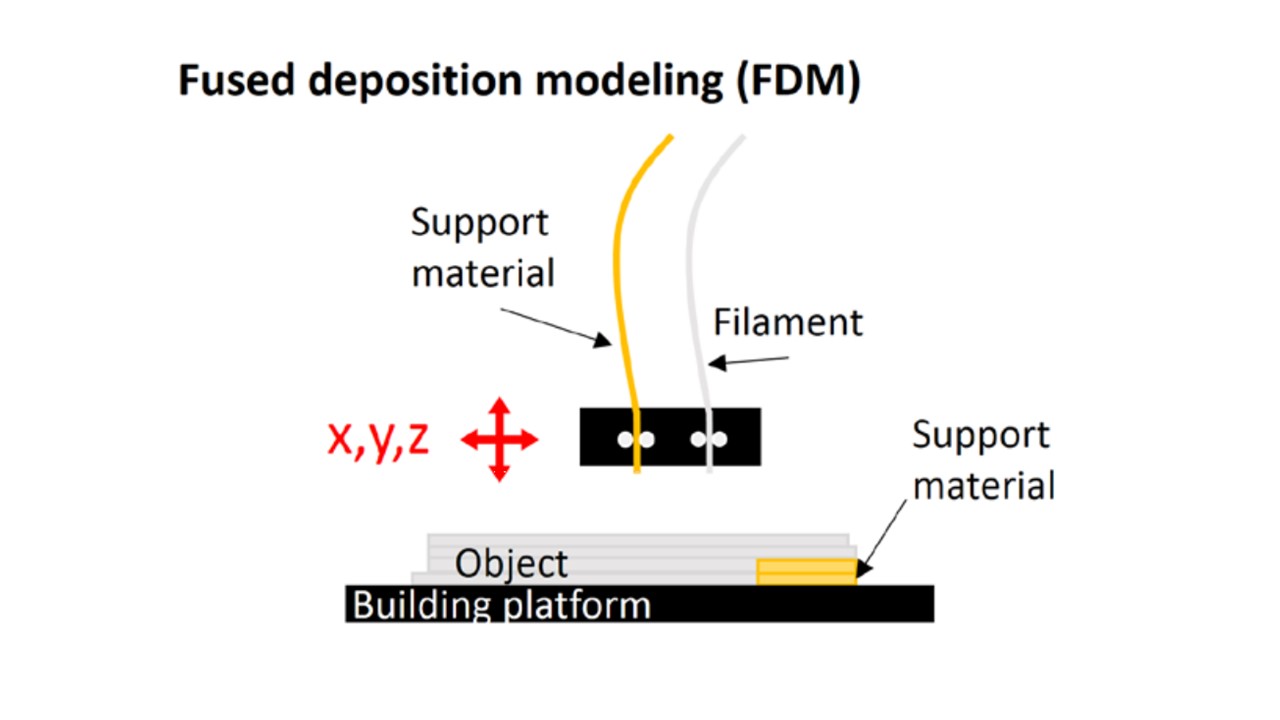
Filaments are melted in fused deposition modelling (FDM) then injected through a nozzle to a bed while cooling and solidifying during extrusion. These printers are inexpensive and fast, but are limited to rigid material. FDM needs a scaffold or bed to support the object during the printing.
Liquid solidification
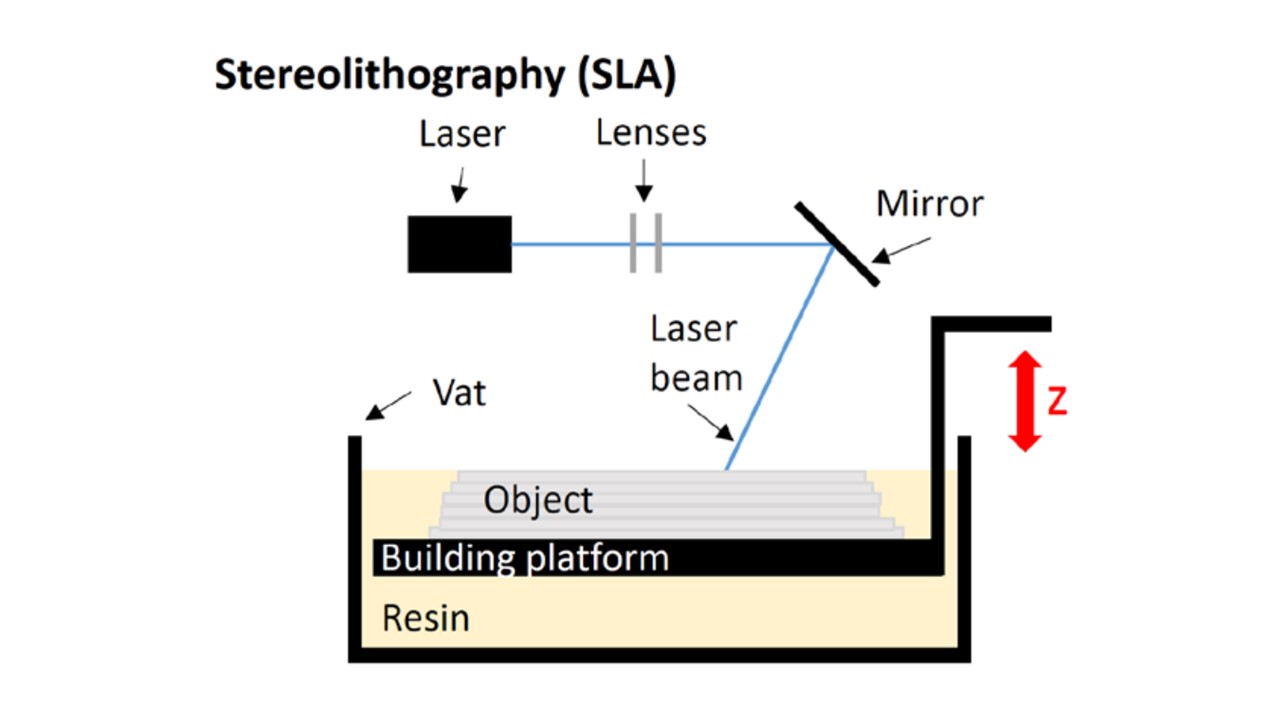
SLA is the oldest method which contains liquid in a vat solidified with an ultraviolet (UV) laser controlled by lenses and mirror reflection, while a building platform is moved down for a layer-by-layer fabrication . A lattice structure is created to support the object.
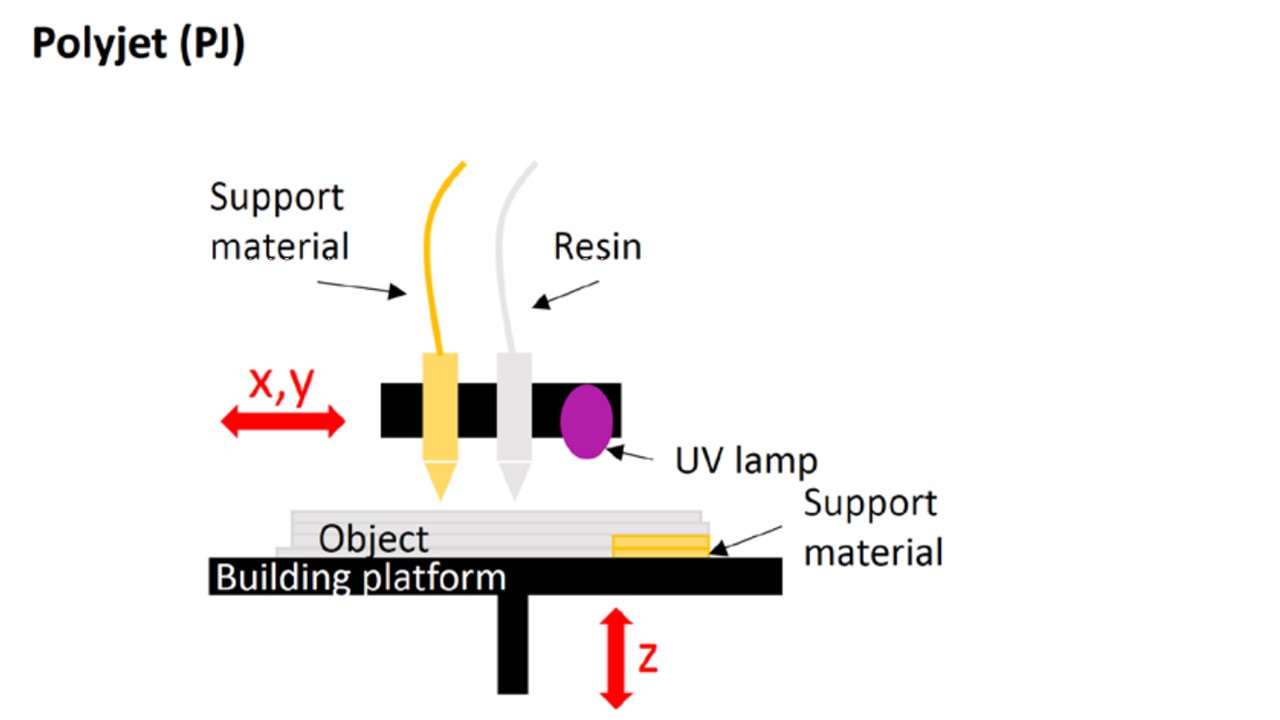
PJ uses jets of liquid to build up thin layers of liquid before UV curing by sliding the head in the x and y axes then a moving platform for the z axis to build up successive layers . PJ is suitable for a wide range of coloured materials with specific properties (eg, rubber-like material).
Powder solidification
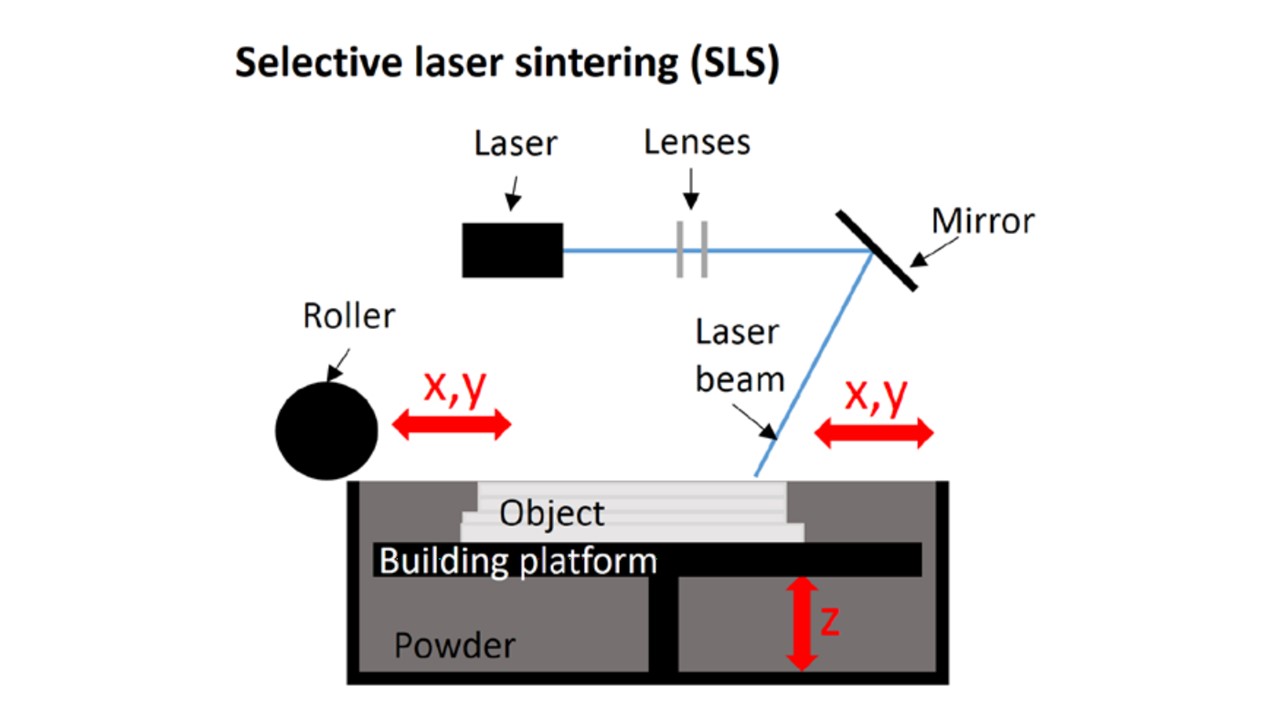
SLS uses a laser to create the surface of an object by sintering a powder. When a layer is done, the build plate is stepping down and covered with a new layer of powder using rollers to keep a constant thickness. At the end of the process, all powder is removed with compressed air and recycled. A wide range of materials are provided for SLS and no scaffold or support material is required since the unsintered powder provides support of the object during the 3D printing.
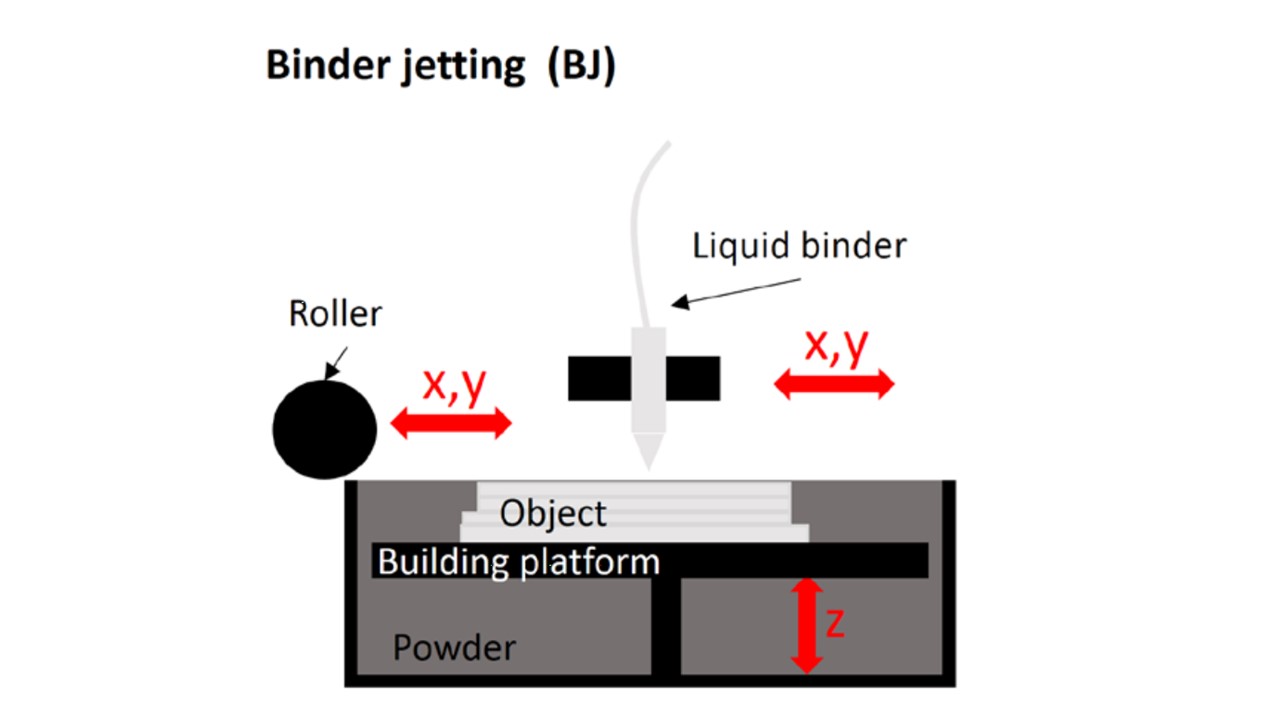
BJ has a platform covered with powder which is moved down while being solidified with a selective spraying of liquid binder; thus, no support material is needed for the fabrication of the object. This technology offers a wide range of materials as far as a powder can be combined with a liquid with enough viscosity to form droplets38. In addition, mechanical properties of the structures obtained by BJ in medical simulation are generally tuned by postprocessing techniques, such as drying and/or heating. Both have an impact on the mechanical properties of
Rigid materials
Human bones are the easiest biological tissues to reproduce by 3D printing as the majority of the materials are rigid. The most common option remains acrylonitrile butadiene styrene (ABS) by FDM but powders of plaster and hydroquinone were also used by BJ, as well as a mix of polyamide with glass beads by SLS.
ABS is the same plastic used in water pipe of most home and is the most affordable material in 3D printing. It has proved to be an appropriate bone substitute with good visual and haptic renderings for practising the drilling with minimised cost, despite the softness of the material.
Flexible materials

Most of the 3D printing materials present a lack of realism to mimic adequately a soft human biological tissue; thus, post processing might be required to soften printed structures. For instance, cartilaginous tissues, for tumours in the context of surgical simulation,arteries to practise transcatheter valve replacements,as well as hepatic segment and hearts
The common techniques to produce this kind of structures are BJ,SLA and PJ (both techniques are previously explained).
Printing with multiple materials
Multimaterial composites may be the future of 3D printed models since none of the current available materials can mimic elastic and biological tissues. Hence, printing materials containing fibres to control adequately the mechanical behaviour of the model are being explored. Mechanical testing can be performed to analyse the biomechanical response of the human tissue by cutting, compressing or tearing apart the material. In this way, multi-material composites may be created based on the capacity of selected materials to mimic the mechanical properties of human tissue.
| Companies | Activity | Country | link website |
| Organovo | Liver Tissue for medicine toxicity testing | USA | link |
| BioBots | Desktop bioprinters | USA | link |
| Cyfuse Biomedical | Desktop bioprinters | USA | link |
| 3D Bioprinting Solutions | Bioprinting human organs | Russia | link |
| Aspect Biosystems | Lab-on-a-Printer platform | Canada | link |
| Materialise NV | Foftware and services | Belgium | link |
| Rokit | Desktop printers | South Korea | link |
| Stratasys | 3D Printers | Israel | link |
| MedPrin | Human tissue repair products | Germany | link |
| Formlabs | 3D Printers | USA | link |
| Institution | Country | Relevant activity | link |
| Massachusetts Institute of Technology | USA | Drug Delivery (info) Devices and Tissue Engineering (info) | link |
| Pennsylvania State University | USA | Cartilage plate (info) | link |
| Wake Forest University | USA | Ears, bones and muscles (info) | link |
| University of Louisville | USA | Capillaries and hearts (info) | link |
| Hospital | 3DP Speciality | Country | Link |
| St. Louis Childrens Hospita | Craniofacial, Cardiology, Nephrology, Orthopedics | USA | Link |
| North Manchester General Hospital | Maxillofacial, Orthopaedic, Anaesthetists | England | link |
| Tan Tock Seng Hospital | Foot Care and Limb | Singapore | link |
| Nicklaus Children’s Hospital | Human hearts | USA | link |
| University Hospital Basel | Cloud-based platform | Switzerland | link |
| Bordeaux University Hospital | Kidney tumor removal | France | link |
| Royal Adelaide Hospital | Craniofacial services | Australia | link |
| Ottawa Hospital | Hand surgery | USA | link |
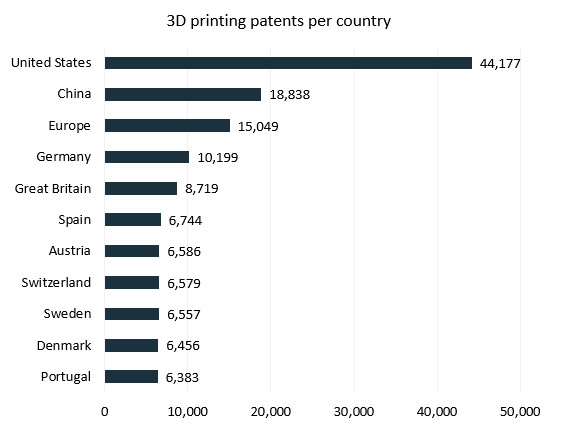
3D printing technology affects virtually all areas of IP law: copyright, patent law, design, law, and even geographical indications. One of the main concerns about 3D printing is that its use makes it technically possible to copy almost any object, with or without the authorization of those who hold rights in that object.
| Strategies | Description |
| Copyright final product | Copyright will protect the originality of a work and the creator’s right to reproduce it. This means that if copies of an original object are 3D printed without authorization, the creator can obtain relief under copyright law. |
| Industrial design rights final product | Industrial design rights protect an object’s ornamental and aesthetic appearance. |
| Patent final product | Patent protects its technical function. prohibit supplying or offering to supply the means to use an invention without authorization. The patent owners should be able to seek redress from third parties for supplying or offering to supply 3D print files on the grounds that these are an “essential element of the invention covered by the patent”. Intellectual Property Code of France (Article L 613-4). |
| Three-dimensional trademark final product | Three-dimensional trademark allows creators to distinguish their products from those of their competitors (and allows consumers to identify its source). |
| Copyright digital file | Copyright of the digital file may be protected under copyright law in the same way that software is. the author of a digital file that is reproduced without authorization could claim a moral right in the work if their authorship is called into question. |
Measures to curb unauthorized use
| Mesure 1 | To mark an object and its associated 3D print file with a unique identifier to monitor use. |
| Masure 2 | Set up a legal offering of downloadable 3D print files or 3D-printed objects through a cloud-based product innovation platform. |

Edu Soler
Science, healthcare and business are the three pillars that drive me nowadays. I love to engage new people in the adventure of healthcare innovation and always keep on learning from them. I am highly motivated with my participation in performing teams worldwide.
All stories by: Edu Soler


Leave a Reply